A Research Paper By Lilly Turner, Lifestyle Coach, SINGAPORE
Lifestyle Medicine Evidence-Based Approach
Lifestyle medicine is a relatively new branch of medicine focused on research, prevention and treatment of chronic disorders attributed to lifestyle factors and preventable causes of death[1].
Lifestyle medicine is an evidence-based approach shown to prevent and treat disease. It treats the underlying cause of disease rather than its symptoms, focusing on lifestyle modifications. The focus is mainly on promoting healthy eating habits and physical activity, having adequate and efficient sleep, building positive social connections and reducing unhealthy habits like tobacco and alcohol abuse[1].
Lifestyle medicine is an interdisciplinary field of internal medicine, psychosocial and neurosciences, public and environmental health, and biology.

The leading causes of mortality and healthcare costs worldwide are chronic diseases; according to the World Health Organization, 80% of heart disease, stroke and type 2 diabetes and 40% of cancer could be prevented, primarily with improvements to diet and lifestyle. The impact of a poor lifestyle is not limited to physical diseases but also increases the risk for mental disorders such as depression and anxiety, which is increasing worldwide[1].
The economic burden of these lifestyle choices is no longer sustainable and impossible to ignore.
How Lifestyle Medicine Can Help? There is a strong body of evidence that practising healthy lifestyle behaviours reduce the risk of chronic disease. Lifestyle medicine focuses on educating and motivating patients to improve the quality of their lives by changing personal habits and behaviours around the use of a whole food plant-predominant dietary lifestyle, regular physical activity, restorative sleep, stress management, avoidance of risky substances, and positive social connection[1, 2].

It is founded on an evidence-based approach to treating and preventing disease by replacing unhealthy behaviours with positive ones.
Key lifestyle medicine principles include prevention strategies that address lifestyle habits, the underlying biological causes and the pathophysiology common to lifestyle-related disorders. As such, lifestyle medicine is an adjunct form of treatment that helps to bridge the best aspects of public health and conventional clinical medicine[2-5].
Addressing lifestyle factors has the potential to reduce the burden of chronic disease to the health system, and increase the quality of life and longevity in the individual.
In addition to prevention, comprehensive lifestyle changes can reverse disease progression. When we address these root determinants of our health, we find that our bodies often have a remarkable capacity to begin healing themselves. This results in significant cost savings because the regenerative and biological mechanisms that control our health and well-being are so efficient once a physiological lifestyle is adopted[3-5].
Health professionals must communicate that there is no doubt about the basic constituents of a healthy lifestyle but physicians often do not counsel patients about healthy behaviours. Lack of training has been identified as one of the barriers[5].
How Coaching Can Help Preventing or Enhancing Lifestyle Medicine?
As previously said, behaviour modification is vital to preventing or enhancing lifestyle-related diseases.
The World Health Organization states that “simply giving information to patients is unlikely to change behaviour; health care providers must understand the psychological principles that underlie self-management training and comprehend that motivating patient requires more than imparting brief information to the patient”[6].
Long-term health behaviour change requires a different approach to acute disease management. To achieve sustainable health behaviours and outcomes, patients need to be supported in behaviour change techniques that promote self-efficacy, self-determination and self-responsibility[7, 8].
Coaching is emerging as a powerful intervention to help patients initiate and maintain the sustainable change that can be critical to recovery practice. The coach approach delivers a patient-centred collaborative partnership to create an engaging and realistic individualized plan[9, 10].
The coaching process builds the psychological skills needed to support lasting change, including mindfulness, self-awareness, self-motivation, resilience, optimism, and self-efficacy[9, 10].
Motivation is generated by supporting patients to evoke their engaging reasons for change and articulate a clear vision of their health goals.
Once the patient is ready to change, they are encouraged to have a curious and flexible mindset of trial and correction, learning, growth and compassion as they are guided towards their goals while connecting to their values and vision.
Patients are supported to build confidence, focusing on strengths as they learn from past failures and successes to overcome barriers and increase facilitators for change.
The study suggested that behaviour change is more likely to be maintained when goals are self-determined, as patients are both motivated to take action and are invested in the result[10].
Several studies compared the efficacy of health coaching with the traditional approach. They show that coaching is capable to:
- Unlock positive self-intrinsic motivation resulting in an efficient adjustment to a healthy lifestyle;
- Improve good behaviours about nutrition, physical activity, weight management or medication adherence;
- Improve training and exercises adherence;
- Increase the levels of motivation and personal satisfaction;
- Improve physical activity, smoking cessation, alcohol reduction and other behaviour change;
- Helps patients gain the knowledge, skills, and confidence to become active participants in their care.
There is evidence from the medical literature that the incorporation of the coaching framework into medical care can improve patient outcomes [ 11-14]. Coaching increases the chance of patients implementing and maintaining health behaviour change.
What Is Behaviour Change?
Behaviour change, in the context of public health, refers to efforts put in place to change people’s actions and attitudes, to prevent disease. Behavioural change is about altering habits and behaviours for the long term.
Making a lasting change in behaviour is rarely a simple process. It usually involves a substantial commitment of time, effort, and emotion.
Researchers have proposed theories to explain how change occurs; one of the best-known approaches to change is the “Stages of Change” or “Transtheoretical Model”, introduced in 1977 by researchers James Prochaska and Carlo DiClementeevolved through studies examining the experiences of smokers who quit on their own with those requiring further treatment[15].
The model suggests five stages of behaviour change but it also underlines that changing behaviour is not a coincidence but instead is a process and different people are in different stages of change and readiness.
The Five Stages Are
- Precontemplation;
- Contemplation
- Preparation
- Action
- Maintenance
The process of implementing and maintaining change is seen to be curved rather than linear with most people regressing to an earlier stage at some point, often through a lapse or relapse[16-18].
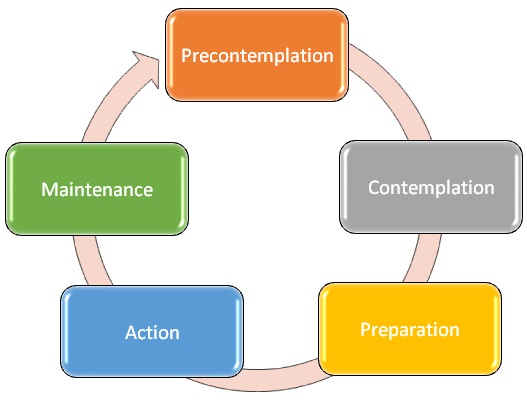
Stage 1: Precontemplation
During the precontemplation stage, clients are not considering a change. Clients in this stage are often described as “in denial,” they might claim that their behaviour is not a problem or there is a lack of confidence in their ability to change, sometimes because of previous failed attempts.
Stage 2: Contemplation
During this stage, clients become more and more aware of the potential benefits of making a change but they are also very aware of the disadvantages and challenges, which can keep them stuck in this stage.
Stage 3: Preparation
During the preparation stage, you might begin making small changes to prepare for a larger life change. Clients’ motivation is strong and they will be planning to implement their change. Within this stage, the client will brainstorm possible approaches and solutions.
Stage 4: Action
During the fourth stage of change, people begin taking direct action to accomplish their goals. Frequently, resolutions fail because the previous steps have not been given enough thought or time. When clients are in this stage, they are likely to “achieve better and quicker results”; this can be encouraged by the coach through the creation of an appropriate, robust and comprehensive action plan.
At this stage, there is also a high risk of lapse or relapse. Reinforcement, support and figuring out potentially challenging situations are extremely important in helping and maintaining positive steps toward change.
Stage 5: Maintenance
The maintenance phase of the Stages of Change model involves successfully avoiding former behaviours and keeping up new behaviours.
Clients are generally confident that they can maintain their new behaviours. However, they will still need to be diligent to maintain this change as lapses can still easily occur, including from risks such as boredom or slowly reverting to their old behaviour.
At this stage, relapse is a common occurrence. When clients go through a relapse, they might experience feelings of failure, disappointment, and frustration.
The key to success is to not let these setbacks undermine their self-confidence instead focus on helping the client to reconnect with the motivators they identified in previous stages including their vision, goals, values and strengths.
Lifestyle Medicine Coaching
Changing behaviours can be a challenging task for all of us. In the context of lifestyle medicine, coaching aims to support individuals living with chronic conditions to adopt sustainable health-promoting behaviours and improve their quality of life. As coaches, we can be part of a lifestyle-oriented medical practice helping clients in changing their unhealthy behaviours making them accountable and active part of their change.
As coaches, we can support them to build self-determination, self-efficacy and motivation. Being empathetic, compassionate and holding a judgement-free approach we can encourage and enable our clients to explore and try out different ideas and opportunities to obtain a change that can be maintained over time.
References
American College of Lifestyle medicine
Mechanick, Jeffrey I.; Kushner, Robert F "The Importance of Healthy Living and Defining Lifestyle Medicine". Lifestyle Medicine: A Manual for Clinical Practice.., eds.
John Wiley & Sons Ltd “Lifestyle medicine potential for reversing a world of chronic disease epidemics: from cell to community”, Int J Clin Pract
Azevedo Da Silva M, Singh-Manoux A, Brunner EJ et al.“Bidirectional association between physical activity and symptoms of anxiety and depression: the Whitehall II study”., Eur J Epidemiol
Jeffrey I. Mechanick, Robert F. Kushner “Lifestyle Medicine: A Manual for Clinical Practice”
World Health Organization. Adherence to long-term therapies: Evidence for action. Geneva: WHO
Ornish D, Scherwitz LW, Billings JH et al. “Intensive lifestyle changes for reversal of coronary heart disease”, JAMA
Ornish D “Avoiding revascularization with lifestyle changes: the multicenter lifestyle demonstration project” Am J Cardiol
Frates, Elizabeth Pegg MD; Moore, Margaret A. MBA; Lopez, Celeste Nicole MD; McMahon, Graham T. MD, MMSc, “Coaching for Behavior Change in Physiatry”, American Journal of Physical Medicine & Rehabilitation
Shivaun Conn, Sharon Curtain. “Health coaching as a lifestyle medicine process in primary care”. AJGP
BasakCinar, Lone Schou. “The role of self-efficacy in health coaching and health education for patients with type 2 diabetes” International Dental Journal
Olsen JM, Nesbitt BJ. Am “Health coaching to improve healthy lifestyle behaviours: an integrative review”. J Health Promot
Thom DH, Willard-Grace R, Hessler D, et al. J Am Board Fam Med “The impact of health coaching on medication adherence in patients with poorly controlled diabetes, hypertension, and/or hyperlipidemia: A randomized control trial.”
Barrett S, Begg S, O’Halloran P, Kingsley M.“Integrated motivational interviewing and cognitive behaviour therapy for lifestyle mediators of overweight and obesity in community-dwelling adults: A systematic review and meta-analyses”.BMC Public Health
Prochaska JO, Diclemente CC Psychother “Transtheoretical therapy: Toward a more integrative model of change”. Theory Res Pract
Prochaska, J. O., Norcross, J. C., &DiClemente, C. C. Applying the stages of change. Psychotherapy in Australia
Prochaska, J. O., DiClemente, C. C., & Norcross, J. C. In search of how people change: Applications to addictive behaviours. Addictions Nursing Network
Moore, M., Highstein, G., Tschannen-Moran, B., &Silverio, G. Coaching behaviour change. Coaching psychology manual